A redback spider bite (from Latrodectus hasseltii) can cause severe localised pain that often radiates, with regional sweating, nausea, and muscle cramps (latrodectism). First aid is cold packs and cleaning the bite—do not use a pressure immobilisation bandage (unlike funnel-web bites). Call Triple Zero (000) for severe symptoms and 13 11 26 for Poisons Information.
Get Properly Trained: Build confidence for real emergencies. Enrol in a nationally recognised first aid course with First Aid Pro to learn spider-bite management, anaphylaxis response and CPR. Book your course today.
Key Takeaways
Essential Information | Action Required |
Identify: Female redback = glossy black body with a red/orange dorsal stripe | Learn key markings; avoid confusing with funnel-webs |
First Aid: Wash with soap/water; apply cold packs in 20-minute cycles | Do NOT use a pressure immobilisation bandage |
Emergency Contacts | 000 for emergencies; 13 11 26 Poisons Information |
High-risk groups: Children, older adults, pregnancy | Seek prompt medical assessment |
Pain can last hours–days; systemic symptoms possible (latrodectism) | Use analgesia as directed; monitor closely |

Redback Spider Identification (Latrodectus hasseltii)
Redback Spider Identification Guide
- Glossy black abdomen with a red or orange dorsal stripe (often hourglass-like ventrally)
- Bulbous abdomen; long, fine legs; body length up to ~10 mm
- Irregular, tangled cobweb in sheltered, dry locations
- Much smaller (2–3 mm)
- Brownish in colour
- Lack bold dorsal stripe
- Rarely cause medically significant bites
- Garden sheds, garages, carports; under outdoor furniture and barbecues
- Letterboxes, fence posts, meter boxes
- Play equipment and toys left outside
- Around outdoor taps, wood piles, retaining walls
- Most active in warm months but present year-round across Australia
Redback vs Funnel-Web: Why First Aid Differs
Correct identification matters because first aid is opposite for these two spiders.
Feature | Redback Spider | Funnel-Web Spider |
Colour | Black with red/orange stripe (female) | Dark brown/black, no stripe |
Size | Female body ~10 mm | 15–35 mm |
Web | Tangled/irregular | Funnel-shaped entrance to a burrow |
Habitat | Dry, sheltered spots near homes | Moist burrows, rockeries, tree roots |
First Aid | Cold packs, no pressure bandage | Pressure immobilisation bandage |
Distribution | Widespread in Australia | Eastern coastal/inland ranges |
If unsure and the spider is a large black spider without a red stripe, treat it as a funnel-web: apply pressure immobilisation and call 000.

What a Redback Spider Bite Looks and Feels Like
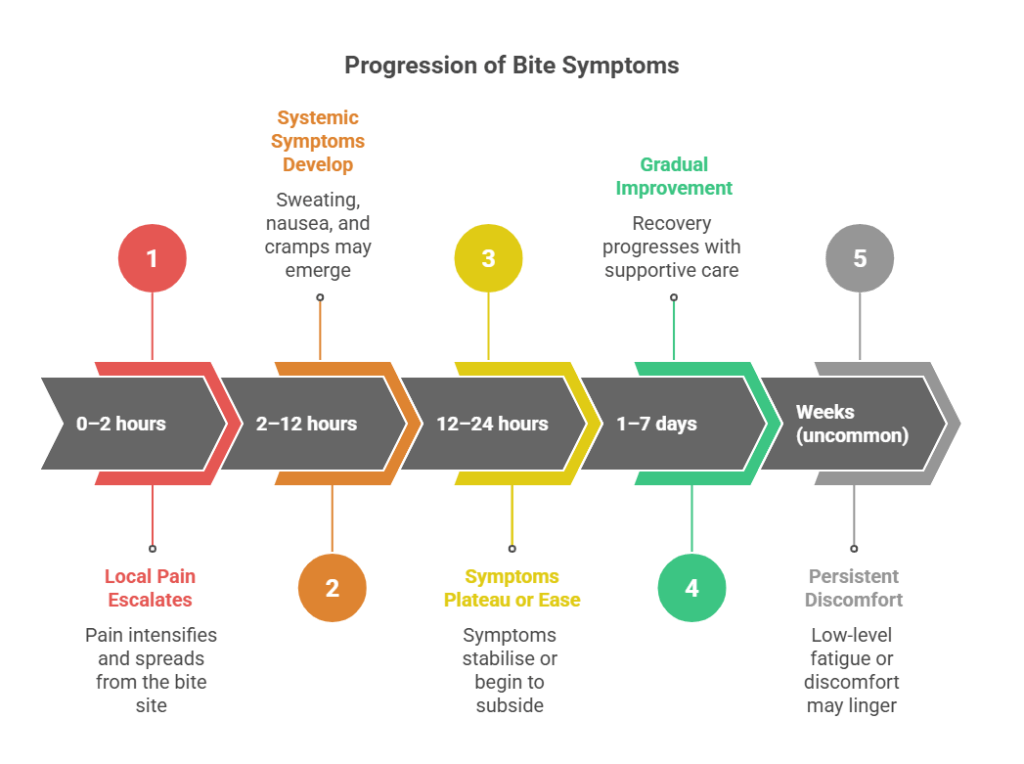
Typical symptom progression from the immediate bite period to systemic latrodectism.
Immediate Symptoms Minutes–Few Hours
- Sharp, burning pain at the site (two puncture marks may be present but are often not visible).
- Local redness and swelling that intensify over 1–3 hours.
- Radiating pain away from the bite.
Latrodectism Systemic Effects
- Regional diaphoresis (sweating localised near the bite).
- Muscle pain or cramping, often in the limb or abdomen.
- Painful lymph nodes (groin or armpit).
- Nausea, vomiting, headache, malaise.
- Abdominal pain/rigidity in more severe cases.
How Long Do Redback Spider Bite Symptoms Last?

First Aid For Redback Spider Bite
First Aid Steps for Redback Spider Bite
Step-by-Step First Aid
- Reassure the person and keep them at rest.
- Wash the bite area with soap and water.
- Apply a cold pack wrapped in cloth for 20 minutes, remove for 20 minutes, then repeat.
- Do NOT apply a pressure immobilisation bandage.
- Call Poisons Information (13 11 26) for tailored advice.
- Monitor for worsening symptoms, especially in children, older adults, and pregnancy.
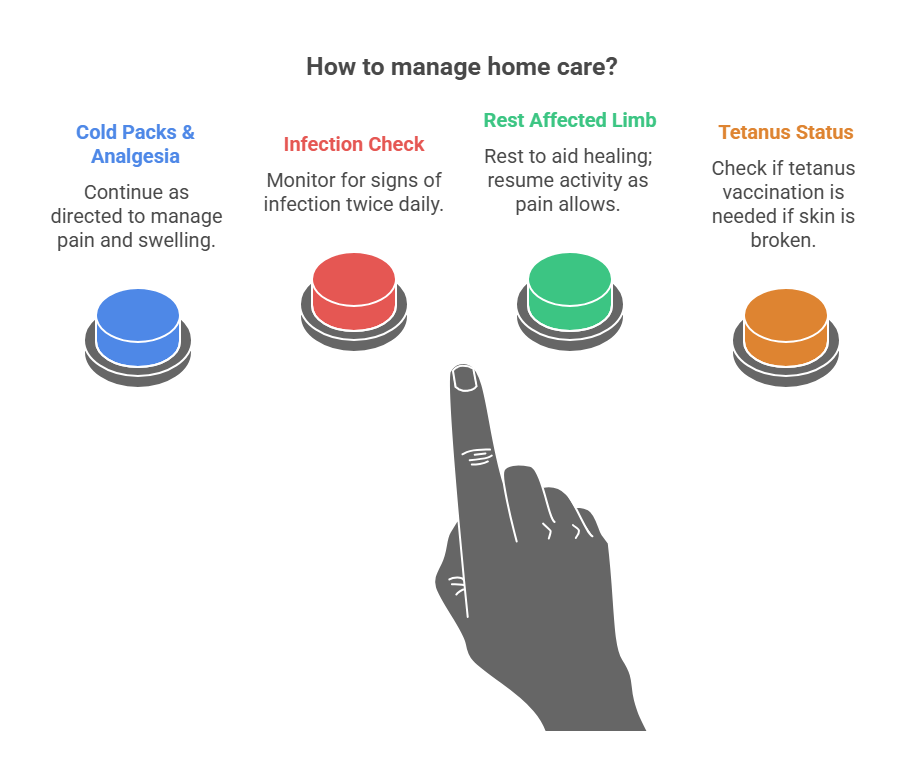
Pain Management & Home Care
- Paracetamol (as directed). Ibuprofen may be considered if appropriate for the person.
- Regular cold packs (20-on/20-off) for pain control.
- Rest and elevate the affected limb.
- Keep the bite clean (gently wash twice daily); watch for infection (increasing redness, warmth, pus, fever).
What Not to Do
- No pressure immobilisation bandage (can worsen pain/tissue injury).
- Don’t cut or suck the bite or apply heat.
- Avoid alcohol or caffeine.
- Don’t leave children or vulnerable people unattended.
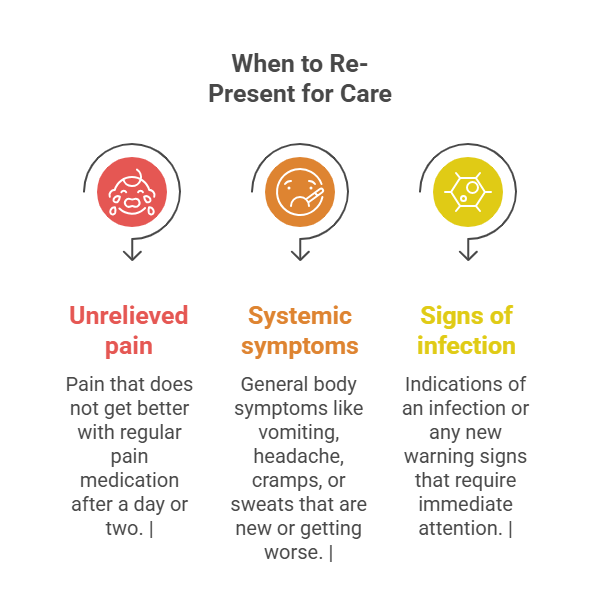
When to Call for Help
Call Triple Zero (000) Immediately If:
- Breathing or swallowing becomes difficult
- Loss of consciousness or collapse
- Severe abdominal or chest pain, or muscle rigidity
- Uncontrollable vomiting or rapidly worsening symptoms
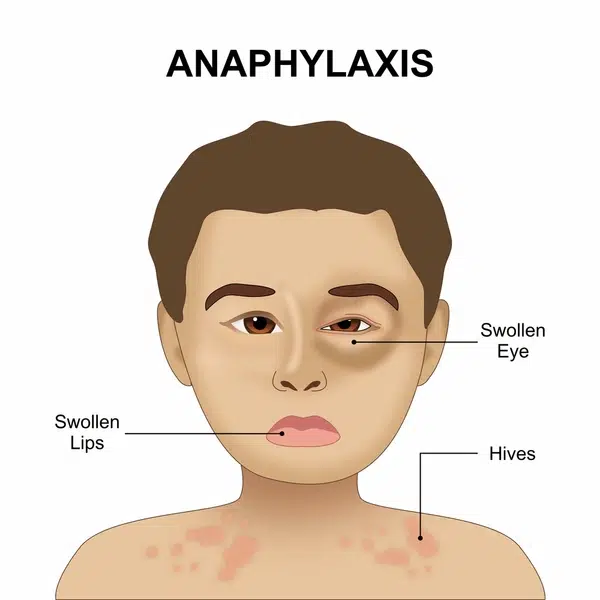
- Signs of anaphylaxis (widespread rash, swelling of face/lips/tongue, difficulty breathing)
Call Poisons Information (13 11 26)
- For any suspected bite to confirm the right first aid and whether to go to hospital
- For children, older adults, pregnancy, or pre-existing health conditions
- If pain persists beyond 24 hours or systemic symptoms develop
Stay Prepared for Emergencies: Learn to recognise anaphylaxis, use adrenaline autoinjectors, and perform CPR. First Aid Pro offers nationally recognised training across Australia. Enrol now.
Special Groups — Extra Care
Children & Toddlers
- All children under 12 with a suspected redback bite should receive medical assessment.
- Symptoms can escalate faster; dehydration from vomiting is a risk.
- Observation in hospital may be recommended.
Pregnancy
- Seek medical evaluation after first aid.
- Some analgesics are contraindicated; consult a clinician.
- Antivenom decisions require specialist input.
Allergies or Chronic Conditions
- People with mast cell disorders, complex cardiac or respiratory disease should seek early medical advice.
- If there’s a known severe allergy, be ready to give an adrenaline autoinjector for anaphylaxis while waiting for an ambulance.
Redback Antivenom & Hospital Care
When a person presents to hospital with a suspected redback spider bite, clinicians will first assess the severity of pain and any systemic symptoms. Treatment typically involves oral or intravenous analgesia to control pain, along with anti-nausea medicines if required. Medical staff will observe vital signs and neurological status closely, while also monitoring the wound for signs of infection.
Redback antivenom has been available in Australia since the 1950s, but current evidence shows mixed benefit in reducing the duration of pain. In many cases, supportive care alone is sufficient. Because allergic reactions to antivenom are possible, its use is now determined on a case-by-case basis, taking into account the severity of symptoms, patient risk factors, and clinical judgement in line with local hospital protocols.
Most patients do not need to be admitted overnight. After several hours of observation and effective pain management, many are safely discharged with clear instructions on wound care, pain relief, and when to return if symptoms worsen.
Recognising Anaphylaxis vs Latrodectism
Feature | Anaphylaxis | Latrodectism (Redback envenomation) |
Onset | Often minutes after exposure | 1–12 hours typical progression |
Skin | Hives, flushing, facial/airway swelling | Usually no widespread hives; local sweating common |
Breathing | Wheeze, stridor, breathing difficulty | Usually normal unless severe pain/anxiety |
Circulation | Dizziness, fainting, hypotension | Pain-related distress; hypotension less typical |
First Aid | Adrenaline autoinjector, call 000, CPR if needed | Cold packs, no pressure bandage, analgesia, call 13 11 26 |
If in doubt and severe symptoms are present, treat as anaphylaxis and call 000.

Prevention: Reduce the Risk at Home
- Declutter sheds/garages; store items off the floor.
- Inspect and clean under outdoor furniture, BBQs, play equipment.
- Use smooth-surfaced letterboxes and furniture that offer fewer hiding spots.
- Trim vegetation away from walls and structures; remove wood piles near living areas.
- Shake out gloves, shoes, towels and covers before use.
- Wear gloves for gardening and when reaching into hidden spaces.
- Seal gaps around baseboards/outbuildings where cobwebs accumulate.
- Lighting in outdoor work areas to reduce surprise encounters.
- Professional pest management for persistent infestations.
Prevention Frequency Table
Location | Prevention Method | Frequency |
Garden sheds | Declutter, sweep webs | Monthly |
Outdoor furniture/BBQs | Check before use, store inverted | Each use |
Letterboxes/fence posts | Smooth-sided designs; quick visual check | Weekly |
Children’s toys/play gear | Store indoors, inspect before play | Daily |
Garage/carport | Organise storage, remove debris | Monthly |
Spiders help control pests; focus on risk reduction in high-use areas rather than eradication.
Aftercare & Recovery

Workplace, School & Childcare Considerations
In workplaces, schools, and childcare settings, it is important to include bites and stings in the organisation’s first aid risk assessment. First aid kits should contain instant cold packs, clean cloths, and soap, with emergency contact numbers such as Triple Zero (000) and the Poisons Information Centre (13 11 26) clearly displayed. Staff must maintain up-to-date training in both general first aid and anaphylaxis management to ensure a prompt and effective response. After any suspected bite involving a child, parents or carers should be provided with clear information about what has occurred and given guidance on symptoms to watch for in the hours that follow.
Build Capability Across Your Team: Book group training with First Aid Pro Adelaide for workplaces and schools—covering HLTAID011 First Aid, HLTAID009 CPR, and anaphylaxis response. Talk to us about onsite delivery.
Knowledge Test Quiz — Redback Spider Bite (Self-Check)
Important Emergency Contacts (Australia)
- Emergency (Police/Fire/Ambulance): 000
- Poisons Information Centre: 13 11 26
- Healthdirect (Non-Emergency Advice): 1800 022 222
From spider bites to anaphylaxis and CPR, the right response saves lives. Enrol with First Aid Pro Adelaide for nationally recognised First Aid and CPR training—online, in-person, or onsite for workplaces and schools. Find a course near you today.
References
- Australian Museum — Spider bites and venoms
- QLD Poisons Information Centre — Bites and Stings
- Perth Children’s Hospital — ED Guideline: Spider Bite
- Healthdirect Australia — Spider bites: Symptoms and treatment
- Charles Darwin University — Spider bite: A current approach to management
- Royal Children’s Hospital Melbourne – Spider Bite – Redback Spider
Please note: Educational only. References are not a substitute for medical advice. Always follow local clinical guidance and seek professional care for concerning symptoms.
Frequently Asked Questions
How can I tell if I have a redback spider bite?
Look for severe, worsening local pain that may radiate, regional sweating, and local redness. If you saw the spider, the female redback has a red/orange stripe on a black abdomen. When in doubt, call 13 11 26.
Should I go straight to hospital after a redback spider bite?
Not always. Start first aid (cold packs, clean the site, no pressure bandage) and call 13 11 26. Call 000 if severe features develop. Children, older adults and pregnancy should be assessed promptly.
Why no pressure immobilisation for a redback spider bite?
Redback venom spreads slowly via lymphatics; pressure techniques can increase pain and tissue injury. Funnel-web bites are the opposite and do require pressure immobilisation.
How long does the pain last after a redback spider bite?
Often 12–24 hours, sometimes several days. If pain is severe or persistent despite proper care, seek medical review.
Are redbacks common in Australia?
Yes—urban and rural environments nationwide. They favour dry, sheltered spots around homes, sheds, and outdoor areas, and can be encountered year-round.